Chief Corner: What's the Deal with Procalcitonin?
/While at UCMC we do not have the option to order procalcitonin (PCT), we do at the VA and it gets ordered all the time - but are we using procalcitonin correctly - and should we be using it at all?
When you search Pubmed for PCT you get 5165 hit - most recently there is an article entitled “Is serum procalcitonin level a reliable indicator in early diagnosis of congenital pneumonia,” and I am not even sure I know what congenital pneumonia is… But, the point is that the use of PCT is strongly debated and you can easily find papers to support whichever position you want, so how do we make heads or tales of the literature?
For anyone who has read The Hitchhikers Guide to the Galaxy - the answer is that we need to find the right question.
There are many questions that are floating around the internet about procalcitonin, but many of the landmark papers about PCT address the following:
Is PCT sensitive and specific enough to differentiate pneumonia from a viral respiratory illness?
Does the clinical use of a PCT guideline decrease antibiotic use without increasing adverse effects
Can you use PCT to stop antibiotics earlier than previous guidelines?
Lets tackle these one-by-one
Is PCT Sensitive for Bacterial Pneumonia?
Note how many patients had no pathogen identified! (62%)
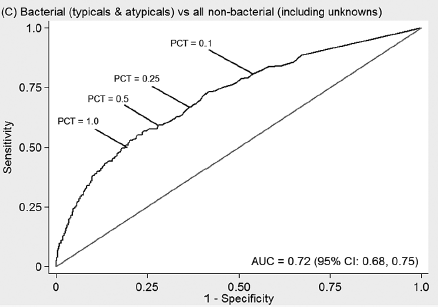
There are many papers that address this question, but most run into the issue that pneumonia is still largely a clinical diagnosis. Self et. al. in Procalcitonin as a Marker of Etiology in Adults Hospitalized with CAP tried to address this by studying PCT levels in people with confirmed bacterial pneumonia through blood cultures, sputum cultures, BAL cultures, urine antigen testing and sputum PCRs. In distinguishing confirmed bacterial pneumonia from all others (viral + unknown), they got an Area Under Curve (AUC) of 0.72 - not great.
When comparing Bacterial vs Non-Bacterial (including unknown etiology) they obtained the following sensitivities: with a cut off of 0.1ng/mL, sensitivity of 81% and specificity of 46%, PPV 19%, NPV 94%, Positive LLR 1.5, Negative LLR 0.41; with a cut off of 0.25ng/mL, sensitivity of 67%, specificity of 63%, PPV 22%, NPV 92%, Positive LLR 1.8, Negative LLR 0.52.
A meta-analysis from 2019 showed a similar sensitivity/specificity and AUC when pooling eight studies that attempted to differentiate bacterial pneumonia from viral pneumonia.
So this begs the question, if PCT only has mild-moderate predictive power in identifying bacterial pneumonia, how could it have any effect on decreasing antibiotic use without increasing adverse effects?
Does PCT Safely Decrease Antibiotic Use?
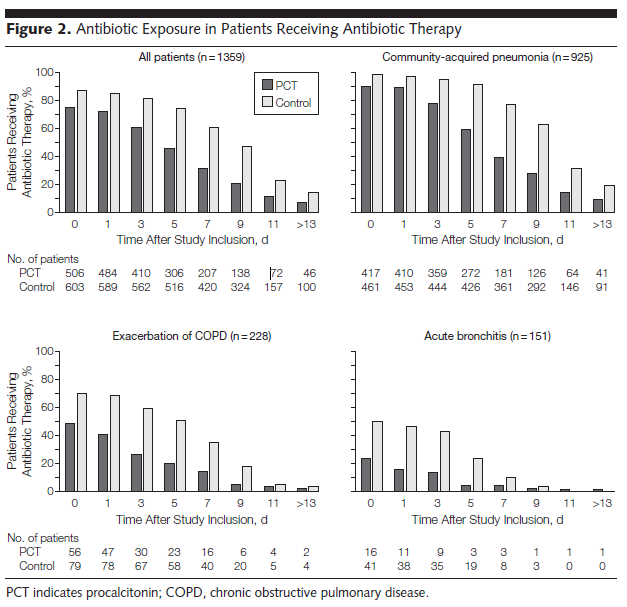
In Europe, Mirjam Christ-Crain authored many of the original papers of antibiotic use and procalcitonin that showed a decrease in antibiotic prescription without increased adverse effects when physicians were obligated to follow strict procalcitonin guidelines. ProHOSP was a European-based large RCT with 6 centers that attempted to answer this question. 1381 patients diagnosed CAP, AECOPD, Acute Bronchitis or other LRTI with were randomized to a strict PCT-guided care vs usual guideline-based care.
They showed that the PCT arm of the trial had significantly fewer antibiotic prescriptions and shorter durations of antibiotics when prescribed without any increase in adverse effects from withholding antibiotics (death, ICU admission, recurrence/rehospitalization, disease-specific complication).
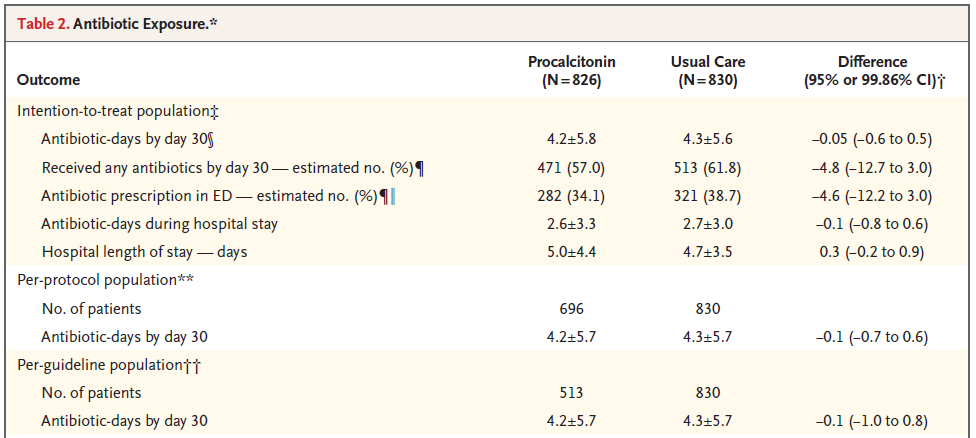
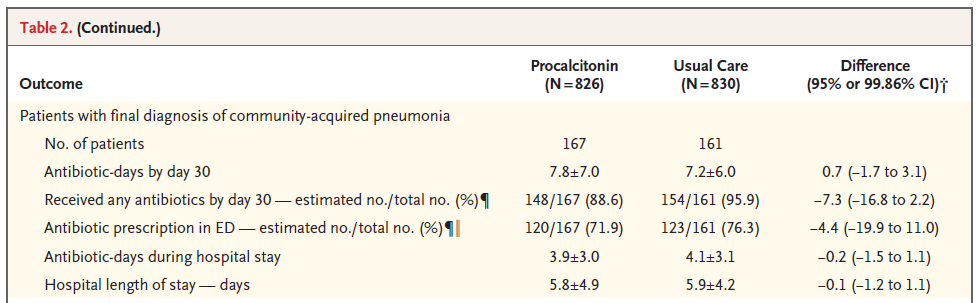
In 2018, ProACT replicated this study with slight modifications in the US with strikingly different results. They randomized 1656 patients to PCT-guided care vs usual care and found no significant different between the two arms of the study with respect to either antibiotic exposure or adverse effects at 30 days.
There were interesting differences between ProHOSP and ProACT - one being the adherence to the protocol. In ProHOSP, the investigators required strict adherence to the protocol with need for documentation of any deviations which cut down on non-adherence. ProACT attempt a “best care scenario” implementation which was not as strict in requiring adherence but recreated how a health system would truly implement a new test like this. Additionally, the rates of CAP in ProHOSP and ProACT were significantly different (nearly 60% vs 20%). Finally, the prescribing habits of the EU vs the US are different making it hard to generalize many of the PCT trials from the EU to the US.
So we have conflicting results on a large population based level…
Can you Safely Use PCT to Discontinue Antibiotics Early?
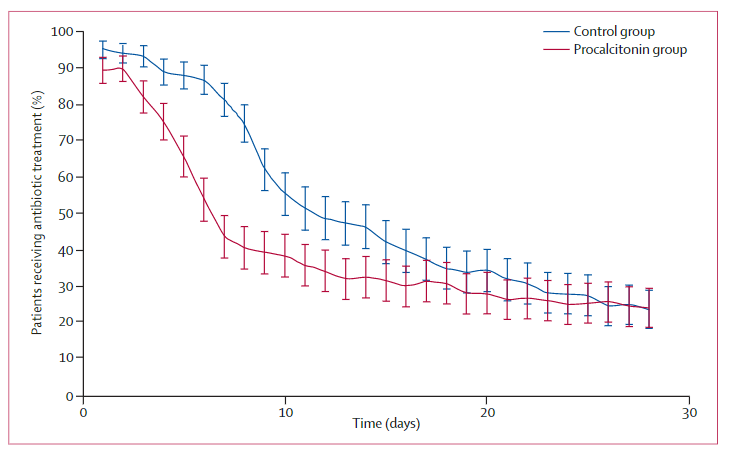
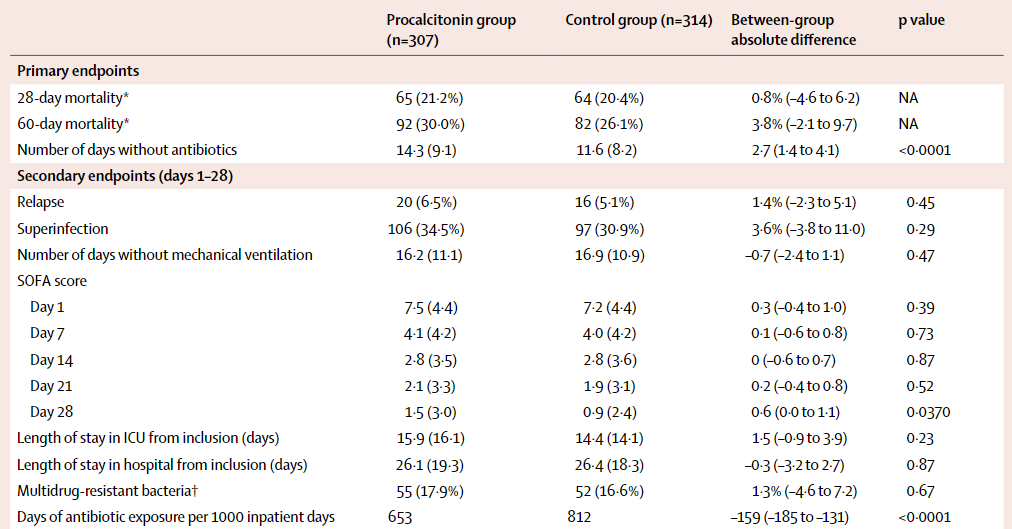
This has been studied extensively and it is far beyond the scope of this article to review all that data, however the largest RCT to look at this was the ProRATA trial from 2010. They randomized ICU patients in septic shock (largely respiratory in origin) to PCT-guided therapy vs usual care. Results showed that they were able to decreased days of antibiotic exposure over the course of the patients’ stays without increasing adverse effects. Looking at the use of antibiotics overtime, it appears that both on day 1 and by day 14 the two arms overlapped in antibiotic use - which begs the question is there any significant benefit from 2.7 fewer days of antibiotics in terms of resistance or adverse effects?
Summary
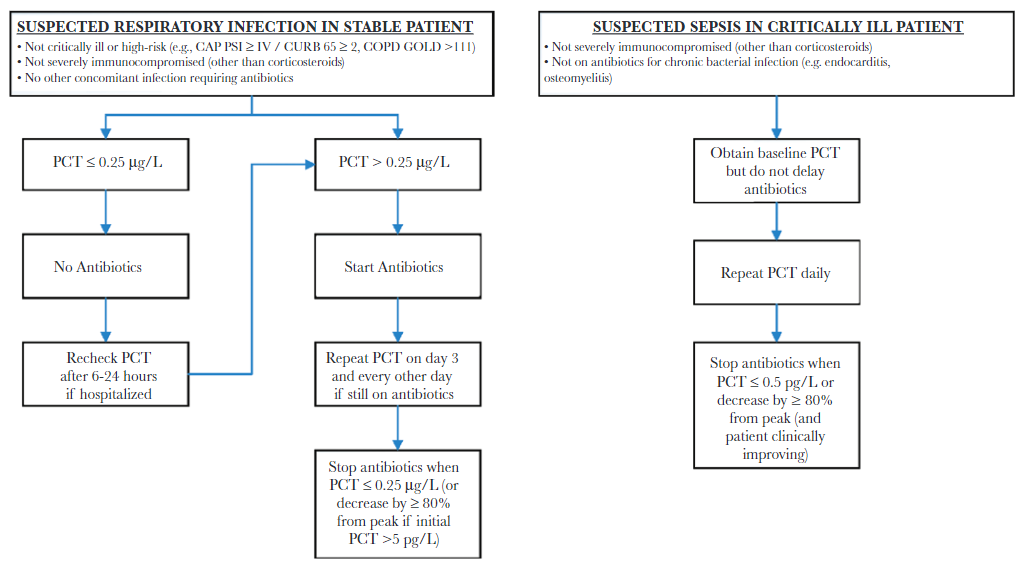
It is hard to summarize a subject with so many view points and articles written about it but I think the key for procalcitonin is to keep in mind the question that is being asked. When asking if PCT can diagnose bacterial pneumonia, the answer is probably not (not with those positive and negative likelihood ratios!). However, when you zoom out from the diagnosis of pneumonia to the clinical implications on a population level, the question changes to “can PCT decrease antibiotic exposure safely?” The answer in this case may be yes. Elevated PCT does not identify all bacterial pneumonia cases, but perhaps it identifies cases which require antibiotics? The issue is that clinical medicine lies somewhere in between individual diagnosis and population outcomes - so the question remains:
How will you use procalcitonin?
When you are ordering it at the VA, try to keep in mind what you are using it for: are you trying to rule out a pneumonia in favor of a heart failure exacerbation? Are you trying to decide if the pneumonia is viral or bacterial? Are you trying to stop antibiotics early?
Finally, to leave you with reviews and meta-analyses from people far smarter:
A recent Cochrane Meta-analysis from 2017 concluded that:
“This updated meta-analysis of individual participant data from 12 countries shows that the use of procalcitonin to guide initiation and duration of antibiotic treatment results in lower risks of mortality, lower antibiotic consumption, and lower risk for antibiotic-related side effects. Results were similar for different clinical settings and types of ARIs, thus supporting the use of procalcitonin in the context of antibiotic stewardship in people with ARIs”
And a recent review article from the IDSA recommended the use of PCT to guide antibiotic therapy.
Gene Novikov, MD